Cartilage Lesions
The surface of the knee joint is coated in a very smooth gliding surface made out of a tissue called hyaline cartilage. This allows the opposing services of the joint to glide over each other effortlessly and with very little friction.
What are cartilage lesions?
Unfortunately this coating can become damaged. Sometimes a twisting or impact force causes some of the cartilage to break away. This in turn can cause symptoms of pain, catching and clicking. Hyaline cartilage does not heal itself very well and this can lead to a permanent defect and problems.
There are a large number of different ways that this can be repaired and the technique chosen depends on the size and location of the defect and also is dependent on any other injuries to the knee.
Not all defects need to be repaired or filled in sometimes the area does not cause any symptoms. If it is relatively small it can heal.

Treatment options
Microfracture
In this technique which is only suitable for relatively small lesions. Small holes are made into the bone under the defect using a wire, drill or special tool. This allows the elements from the bone marrow in the bone which contain stem cells to flow into the defect and form a ceiling type of cartilage called fibrocartilage. This type of cartilage is not as good as the native cartilage but can give good pain relief for small areas although sometimes the repair area can fail with time. This procedure can be performed with key hole surgery.
Osteotomy
If the damaged area occurs in the knee joint where the alignment is causing increased loading to that area and osteotomy is often performed as well as or instead of any of the above procedures. The osteotomies is a procedure to change the alarm into the leg so that less weight is placed through the affected part.There is a separate section dedicated to this treatment on my website.
I am able to perform all of the above techniques. There is no one correct treatment. therefore at your consultation I would discuss the treatment options available to us, pro’s and cons of each option and come up with a treatment plan best suited to your own circumstances.
Augmented microfracture (AMIC)
This technique is similar to the above however in addition to making holes in the bone a special membrane is attached to the defect with sutures or biological glue. This acts as a patch to hold the healing elements in place. It is more successful for treating larger areas of damage. This procedure is performed keyhole or open depending on size and location of the defect.
Osteochondral Allograft
This technique is suitable for larger injuries and defects to the joint surface. A piece of bone and it’s overlying hyaline cartilage is taken from a cadaver after it has been thoroughly screened to ensure it doesn’t contain any infection or disease. The donated tissue has to be specifically matched for size and shape to the specific defect it is required to fill. An open procedure is used to attach the donated tissue into the defect usually in a press fit manner.
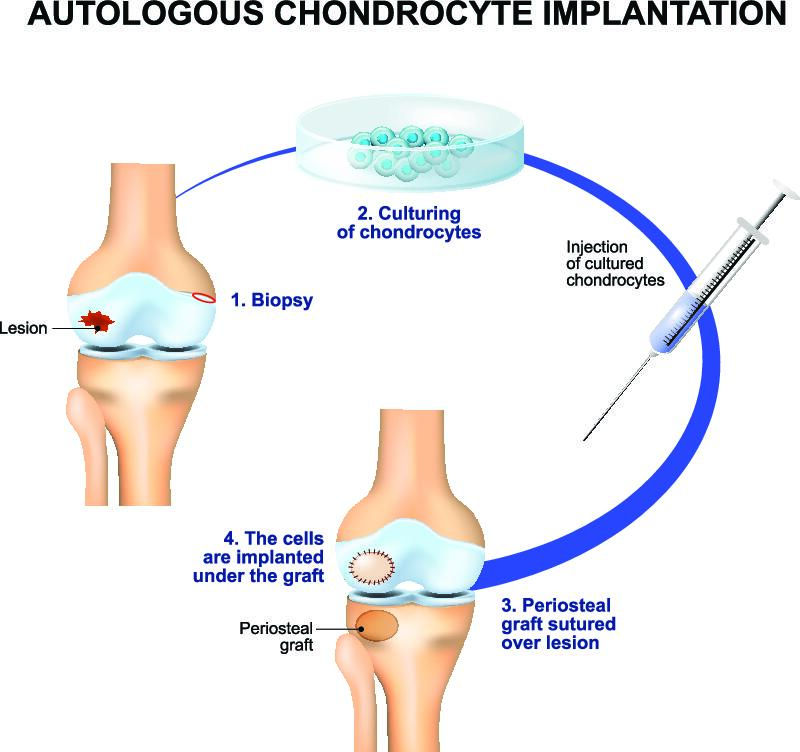
Autologous Chondrocyte Implantation
This technique is the gold standard for treatment of cartilage defect in the knee. It is however a two-stage procedure. Healthy cartilage cells from the less important area of the knee are harvested in an initial operation. They are then grown in a laboratory to increase their number and size and seeded onto a membrane that can be inserted into the defect. In a second procedure the membrane is attached to the defect. This technique is very expensive and as a result it’s not covered by some of the insurance companies and in the UK it’s difficult to perform because of a lack of company is currently growing the cells required. The technique is also dependent on a very long rehabilitation and regime.
Focal Resurfacing Implants
Recently a number of different types of small implants have been developed to fill or resurface defects in the knee joint. These are usually metallic or plastic implants that have been specifically shaped for the area and are inserted into the vision via a peg or screw. These are not made of biological tissue giving them the benefit of a faster recovery but they are also subject to wear or could potentially where other parts of the knee joint. They have demonstrated very good short-term results but as they haven’t been used for a long period of time we do not know what the long-term rates of where the Phalia are. One such implant is called the Episealer. It is custom made for a specific defect and patient by using a pre-operative CT scan and then a 3-D printed implant is made to exactly fit the injured area.
Get in touch
Get in touch with us today using the contact form to book a consultation.


